Scientists at Southern Research’s Drug Discovery division have joined the fight against malaria through efforts aimed at discovering new drugs and improving the safety and efficacy of current antimalarial medicines.
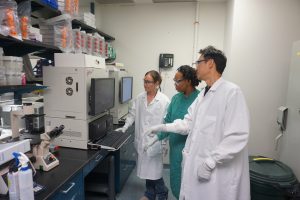
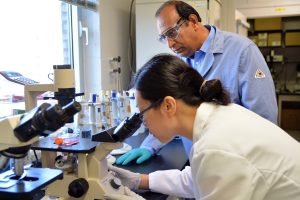
A research team lead by Babu Tekwani, Ph.D., distinguished fellow and chair of the Department of Infectious Diseases at Southern Research, is working on the development of nano-formulations of drugs that prevent relapse of the illness.
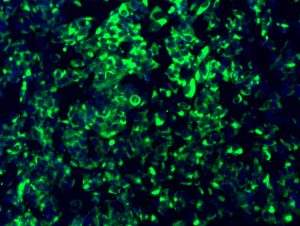
This project, funded by the NIH’s National Institute of Allergy and Infectious Diseases (NIAID), targets malaria caused by Plasmodium vivax, one of the five plasmodium parasites responsible for the serious and sometimes fatal disease in humans.
Vivax malaria is notorious for causing relapses, even after treatment with commonly used antimalarial drugs.

Today, Primaquine is the only FDA-approved drug available to prevent relapses in malaria patients, eliminating all malaria parasites from the body in what is referred to as radical cure.
The medicine, however, causes severe destruction of red blood cells, a condition known as hemolysis, in individuals with the genetic deficiency of glucose 6-phosphate dehydrogenase (G6PD).
This side effect prevents the use of Primaquine in a substantial proportion of malaria-infected individuals.
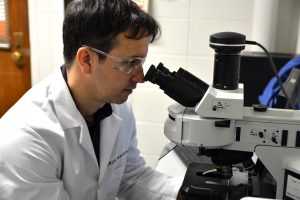
Tekwani’s team at Birmingham-based Southern Research has established specific experimental models and bioassays to evaluate the safety and efficacy of drugs in G6PD deficiency. These models are being employed to test new antimalarial drugs and formulations.
Tekwani’s team is also working on a research project to better understand the molecular basis of antimalarial drugs’ action. The goal of the project is to develop new antimalarial drugs with better safety profiles and activity against drug-resistant cases of malaria.
This project is funded by the U.S. Department of Defense in collaboration with the University of Mississippi and the Walter Reed Army Institute of Research.
“The continuous emergence of drug-resistant cases of malaria underscores the need for the identification of new drugs,” Tekwani said. “Indeed, the building and continuous augmentation of an armamentarium of multiple drugs is necessary to cope with the growing problem of drug-resistance”.
“The experimental models we’ve developed for evaluation of the safety and efficacy of antimalarial drugs have provided better tools for new antimalarial drug discovery,” he added.
BATTLING MALARIA
Malaria continues to be a global health challenge despite extensive efforts initiated by global and public health agencies for malaria control. The mosquito-borne disease claimed the lives of 435,000 people in 2017, of which included mostly children in Africa. There were 219 million cases reported worldwide that year. In addition, an estimated 1,700 cases of malaria are reported in the U.S. each year.
More than 3.3 billion people in 106 countries continue to be at risk for contracting malaria, according to a 2018 world malaria report published by the World Health Organization (WHO).
Extensive efforts initiated in 2000 by malaria-affected countries and global health agencies have led to remarkable progress in reducing malaria-related deaths from more than one million to less than 500,000 per year. However, progress has been stagnant since 2015, and malaria is even re-emerging in some countries.
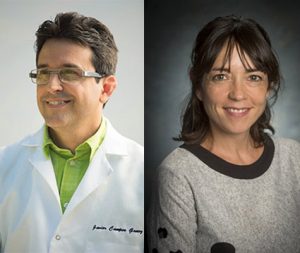
“Southern Research is looking forward to making important new contributions to malaria drug discovery with the extensive experience of Dr. Tekwani in this area and funding from the NIH-NIAID and the U.S. Department of Defense,” said Mark Suto, Ph.D., vice president of Drug Discovery at Southern Research.
The Department of Infectious Diseases in Southern Research’s Drug Discovery division focuses on a diverse array of infectious disease pathogens, with the objective of identifying novel mechanisms, targets and strategies for the prevention and treatment of protozoal, bacterial and viral infectious diseases throughout the world.
Tekwani has spent more than 30 years researching tropical parasitic diseases such as malaria, leishmaniasis and human African trypanosomiasis, vector-borne infectious diseases and major global health threats. His work on new drug discovery for infectious diseases has identified potential new targets and sources for therapies.




 Tekwani’s research has been funded by the
Tekwani’s research has been funded by the